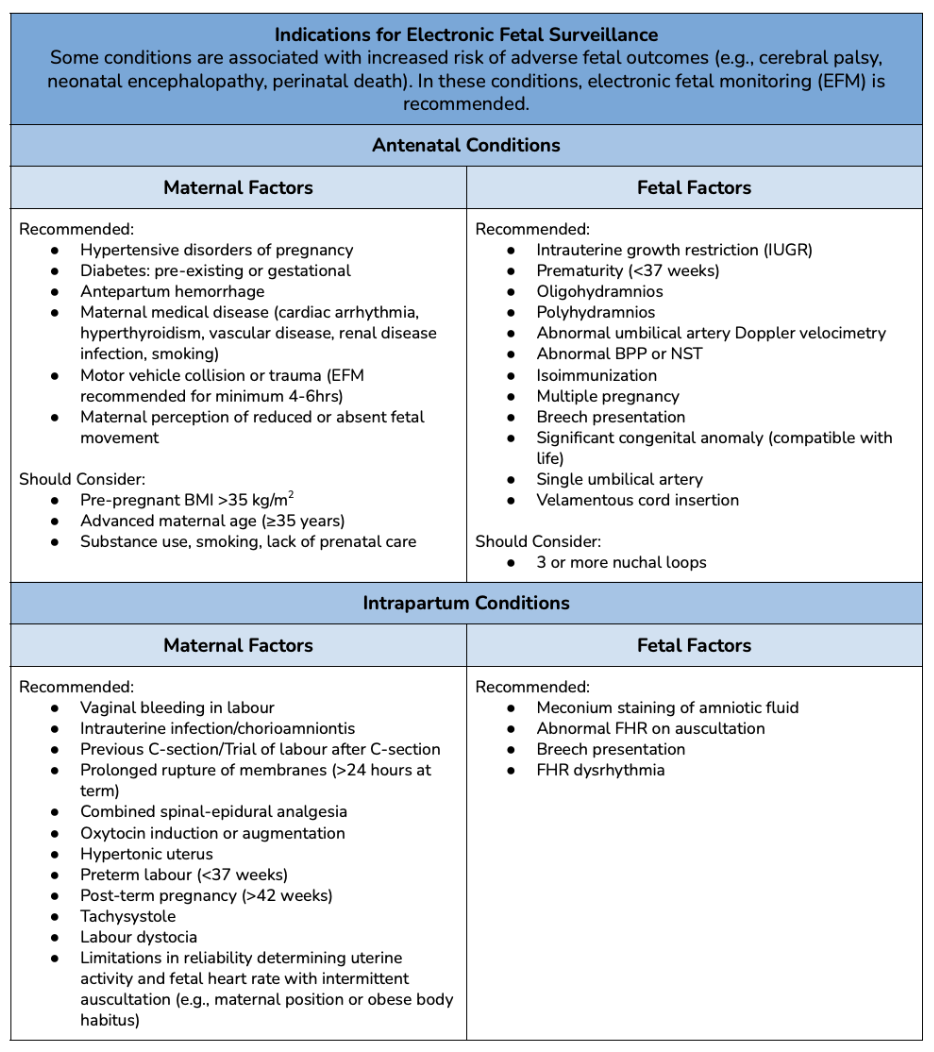
Learners will manage an obstetrical complication of placental abruption and eclampsia.
You’re working in a rural 1A maternity site (no local cesarean section capabilities), and the nearest urban centre is 370 km away. It’s been a quiet morning and your phone starts to ring. It’s your neighbour and she sounds panicked. “It’s my cousin, Canella, she’s not supposed to be due for another four weeks, but she’s been bleeding and doesn’t look too good. We’ll be at the hospital shortly.”
Your neighbour’s 41 y/o cousin presents to the ED at approximately 36 weeks gestation with significant vaginal bleeding. She’s been having intense cramps and abdominal pain that she rated 9/10. She also states that she has “noticed less movement” from the fetus over the past few days. She appears to be pale, lethargic, and confused.
She’s had a normal prenatal course, has been well throughout her pregnancy, is multiparous (four children), and is carrying a singleton pregnancy. Prenatal labs are not available. Her past medical history is insignificant except for a history of preeclampsia in two of her past pregnancies. She has no allergies and only takes low-dose aspirin (81 mg) daily. She smokes one pack of cigarettes per day.
On examination, the learner will recognize and manage placental abruption and eclampsia. The learner will also demonstrate an understanding of fetal heart monitoring and navigating resource shortages while practicing a massive hemorrhage protocol.
This simulation is part of ØRECLESS (Rural Emergencies and Complications in Labour Events Simulations Suite).
Overall Goal: Manage an obstetrical complication of placental abruption and eclampsia while demonstrating an understanding of fetal heart rate monitoring and clinical decision-making during maternal hemodynamic instability.
Specific Learning Objectives:
Time Recommended: 60 minutes total (10 min Setup | 20 min Scenario | 30 min Debrief)
Patient Recommendation: Standardized Patient + OB Mannequin + OB Trainer
Medical Equipment:
Medications:
Other:
Obstetric Hemorrhage Equipment Tray (Extra Information/ NOT required for SIM):
Access/exposure:
Eye Needles:
Sutures:
Uterine/vaginal Tamponade:
|
This SIM requires one learner. Supporting roles can (1) be assigned to complete tasks by the learner, (2) provide assistance with maneuvers, and (3) provide statements throughout the SIM to allow for progression through the stages.
|
Moulage: Task trainer set up with the fetus in cephalic presentation, right occiput anterior position, and fetal station of -2.
Set-Up: The woman walks into the ED with your neighbour. The woman is presenting with persistent vaginal bleeding and abdominal pain.
Note: While prepping for your simulation, don't forget to prep for the debrief. Become comfortable with your chosen framework, review your objectives. For additional debriefing resources, see our Resources page.
Original Author: Tiana Bressan
Originally published on: October 17, 2023
Most Recent Modification: October 17, 2023
A good prebriefing is an essential component of running effective simulations, as it sets the stage for everything that comes after it1-3. An effective prebrief will create a safe container for learning, and in doing so, help participants feel more comfortable pushing their limits, sharing their thoughts and feelings, and buying into the experience. In turn, this will enhance engagement, participation, and learning. To that end, the prebriefing process needs to cover a lot of information1-5, which can make it daunting to novice or non-expert facilitators. To help, we have consulted the relevant literature and put together a prebrief guide to ensure that you have the tools you need to run an effective pre-briefing session.
Throughout the pre-brief, it is important that you convey your commitment to respecting learners and their perspective2-4, and establish and maintain the simulation as a safe space for learning1,4,5.
Prebrief Guide (Sample Phrases in Italics)
Welcome learners. Introduce yourself, your role, and your experience with simulation.
Go over the time requirements for the simulation, when breaks will occur, how learners should handle incoming calls or texts, etc.
Clarify the learning objectives for the simulation1-5. Give information on the purpose of the simulation without giving out specific actions or information that might compromise the learning experience for participants.
Explain how participants will be evaluated (formative/summative/not evaluated). Briefly discuss the debrief process that will take place at the end of the simulation.
Give details on what expectations are for the learners' behaviour during the simulation, setting basic ground rules2-5. Go over expectations for yourself as the facilitator. Reinforce the simulation as a learning environment, where mistakes aren't something to be punished but opportunities for further learning.
This could be a good place to pause and ask learners if they have any additional expectations, fears, comments, or questions about the topic for the day.
Ensure all participants agree to the confidentiality expectations of the simulation. Often, this will follow the mantra of "What happens in the simulation stays in the simulation," where learners and instructors agree not to share information on others' performance or scenario details outside of the simulation environment.
Explain that you've done what you can to make the simulation as real as possible, but acknowledge the limitations. Ask the learner to commit to doing what they can to act as if everything was real, explaining that the quality of their learning will depend on their willingness to participate as fully as possible. For the first simulation with a new group, it could be helpful to explain the importance of a mutual fiction contract.
Explain the different roles in the simulation and assign learners to them. If you have predetermined scripts for certain roles, hand them out here.
Explain the resources that will be available for the participants to use, how they should call for help in the simulation, what your role will be in providing information.
Orient participants to simulation space, equipment, manikin, etc. This can also be done by allowing participants to explore the simulation space and manikin for themselves.
Ask for questions!
References
1. Rudolph JW, Raemer DB, Simon R. Establishing a safe container for learning in simulation: the role of the presimulation briefing. Simul Healthc. 2014 Dec;9(6):339-49. doi: 10.1097/SIH.0000000000000047. PMID: 25188485.
2. Leigh G, Steuben F. Setting Learners up for Success: Presimulation and Prebriefing Strategies. Teaching and Learning in Nursing. 2018; 13(3):185-189. https://doi.org/10.1016/j.teln.2018.03.004
3. Lecomte F, Jaffrelot M. Chapter 33 - Prebriefing and Briefing. Clinical Simulation. 2019; 2nd ed.; 471-482. https://doi.org/10.1016/B978-0-12-815657-5.00034-6.
4. INACSL Standards Committee (2016, December). INACSL standards of best practice: SimulationSM Facilitation. Clinical Simulation in Nursing, 12(S), S16-S20. http://dx.doi.org/10.1016/j.ecns.2016.09.007.
5. Simon R, Raemer D, Rudolph J. Rater's handbook for the Debriefing Assessment for Simulation in Healthcare (DASH) Rater Version. 2009. http://www.harvardmedsim.org/debriefing-assesment-simulation-healthcare.php.
You’re working in a rural 1A maternity site (no local cesarean section capabilities), and the nearest urban centre is 370 km away. It’s been a quiet morning and your phone starts to ring. It’s your neighbour and she sounds panicked. “It’s my cousin, Canella, she’s not supposed to be due for another four weeks, but she’s been bleeding and doesn’t look too good. We’ll be at the hospital shortly.”
Your neighbour’s 41 y/o cousin presents to the ED at approximately 36 weeks gestation with significant vaginal bleeding. She’s been having intense cramps and abdominal pain that she rated 9/10. She also states that she has “noticed less movement” from the fetus over the past few days. She appears to be pale, lethargic, and confused.
She’s had a normal prenatal course, has been well throughout her pregnancy, is multiparous (four children), and is carrying a singleton pregnancy. Prenatal labs are not available. Her past medical history is insignificant except for a history of preeclampsia in two of her past pregnancies. She has no allergies and only takes low-dose aspirin (81 mg) daily. She smokes one pack of cigarettes per day.
|
Patient Chart |
||||||||||
|
Name: Canella Perez |
Age: 41 |
Gender: F |
Weight: 64.5 kg |
Height: 157 cm |
GA: 36 Weeks |
|||||
|
Temp: 35.9 |
HR: 123 bpm |
BP: 107/72 |
RR: 32/min |
O2Sat: 86% |
GCS: 15 |
|||||
| Presenting complaint: Significant vaginal bleeding and abdominal pain. | ||||||||||
Your neighbour's pregnant cousin who is almost full-term arrives at the ED with persistent vaginal bleeding and abdominal pain.
Modifiers (in red): Actions by the learner (which will have a consequence) OR actions to prompt learner. Extra information, audio clips, etc. are provided below.
| Patient Vitals | ||||
| BP: 107/72 | HR (Rhythm): 123 bpm (Sinus Tachycardia) | RR: 32/min. | ||
| O2SAT: 86% | Temperature: 35.9 degrees Celsius | GCS: 15 | ||
| Expected Learner Actions |
|---|
|
Call nursing/staff to increase available team numbers Administer Oxygen (2L/min, Non-Rebreather Mask or Nasal Prongs) Estimate blood loss Administer Tranexamic Acid, 1g IV (100mg/mL at a rate of 1mL/min = 10mL over 10min); repeat if bleeding persists after 30 min or restarts after 24 hours Call for and transfuse 2U pRBC IV (consider pressure bag) Note: Woman is Rh negative Initiate contact with referral centre specialist (e.g., Ontario - CritiCall) Initiate contact with Air Ambulance Service (e.g., Ontario - Ornge) Initiate contact with nearby hospitals for pRBC (O-Negative) Inform the woman of the current situation and management plan |
| 15 min. OR Actions Complete ⇒ 2. Eclampsia |
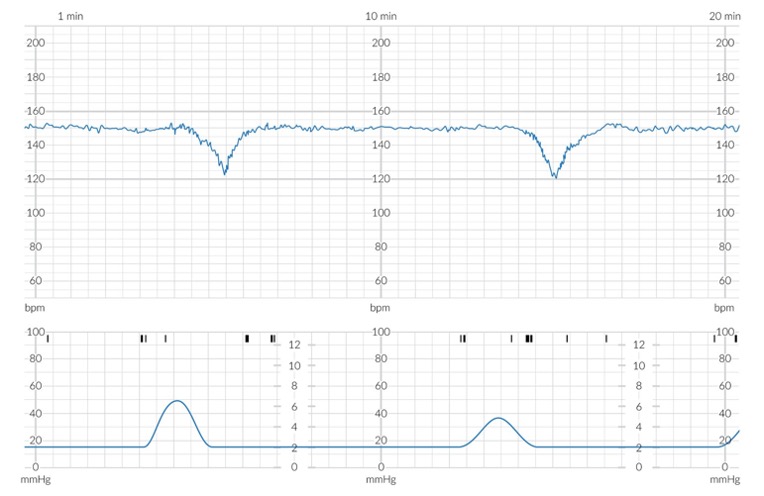
Variability: Minimal, <6bpm (Normal Range = 6-25bpm)
FHR: 150bpm (Normal Range = 120-160bpm)
Heart Tracing: Late Decelerations
Classification: Abnormal
Retrieved July 5, 2023, from https://www.amboss.com/us/knowledge/normal-labor-and-delivery/
Pronouns: She/her
History of Presenting Illness (HPI):
Pregnancy Records: Normal, no complications. Rh. negative.
Gestation: 36 Weeks
Membrane: N/A
No. previous deliveries: Multiparous (G5P4)
Pregnancy Complications: History of preeclampsia in two of her past pregnancies.
Medication(s): Aspirin, 81mg PO qd
Other: No Allergies. Insignificant family history and past medical history. Smokes one pack of cigarettes/day (15 pack years).
General Abdominal Exam: No visible asymmetry, lesions, or scars. No appreciable masses, swelling, rigidity, or guarding. Woman appears to be almost full-term.
Leopold Maneuvers:
Fundal Grip: Palpable soft, irregular mass.
Lateral Grip: Fetal back is on the right side and the limbs are felt on the left.
Pelvic Grip: Head is palpable.
Fetal Lie: Longitudinal
Fetal Presentation: Cephalic
Position: Right Occiput Anterior (ROA)
Uterine Activity Characteristics:
Frequency: Every 5 min. (~2 contractions/ 10 minutes)
Duration: 60 sec.
Intensity: Mild
Resting tone: Rigid between contractions
Dilation: ~3cm (size of a banana slice)
Fetal Station: -2
Effacement: 80%
Copious vaginal blood.
Dilation: ~3 cm (size of a banana slice)
Fetal Station: -2
Effacement: 80%
Copious vaginal blood.
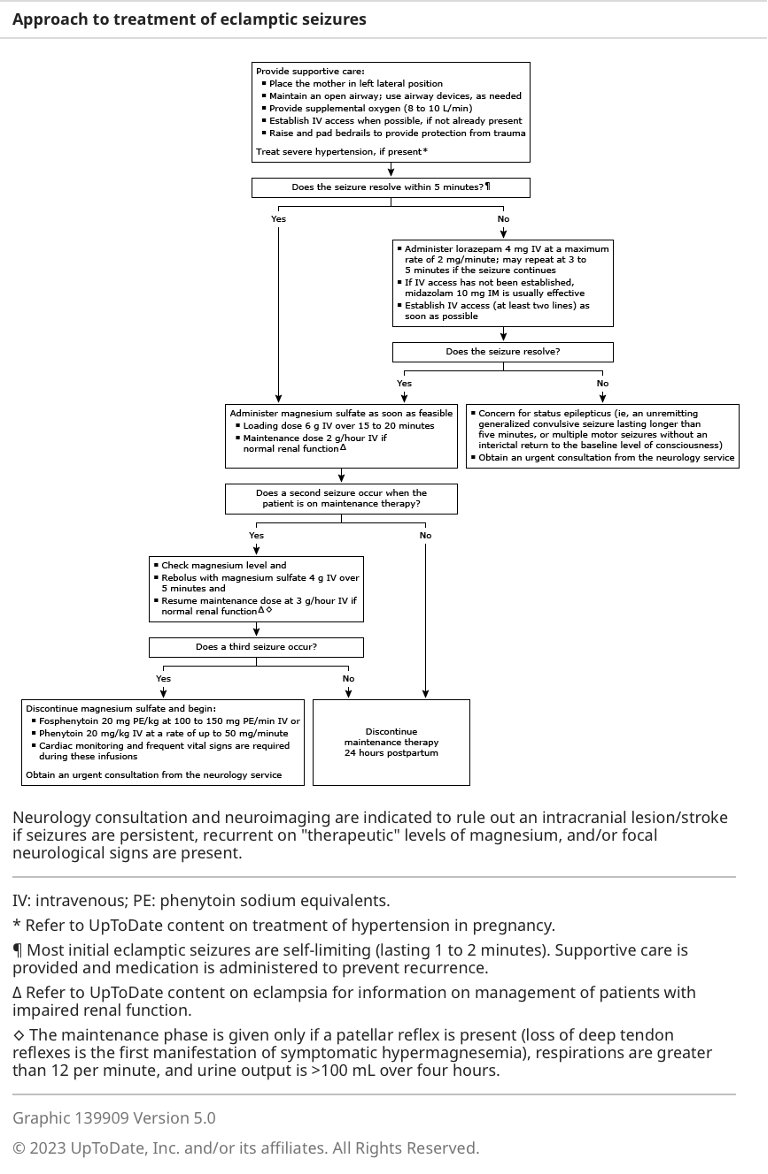
You have followed the massive hemorrhage protocol to maintain maternal hemodynamic stability. The woman begins to seize on the hospital bed.
Modifiers (in red): Actions by the learner (which will have a consequence) OR actions to prompt learner. Extra information, audio clips, etc. are provided below.
| Expected Learner Actions |
|---|
|
Protect the airway (head-tilt chin-life maneuver) |
| 5 min. OR Actions Complete ⇒ 3. Case Complete |
Dilation: ~3 cm (size of a banana slice)
Fetal Station: -2
Effacement: 80%
Copious vaginal blood.
Dilation: ~3 cm (size of a banana slice)
Fetal Station: -2
Effacement: 80%
Copious vaginal blood.
The Air Ambulance Service has arrived and the case is complete.
At this time, you may quantify the blood loss and compare it to the learner's estimate. Subtract the dry weight of the towels from the "blood" soaked towels provided earlier (1g weight = 1mL blood loss).

Retrieved July 2, 2023 from: https://www.parents.com/pregnancy/giving-birth/labor-and-delivery/cervix-dilation-chart-pictures-that-explain-the-stages-of-labor/

Retrieved July 27, 2023 from: https://www.instagram.com/p/CHJCbAhgdIu/?utm_source=ig_web_button_share_sheet
Retrieved July 27, 2023 from: https://www.youtube.com/watch?v=x17vY7_3M2M

Adapted September 12, 2023 from https://www.medicalnewstoday.com/articles/326380

Reference(s):
Society of Obstetricians and Gynecologists of Canada. ALARM Manual, 28th Ed. 2022.

Classification of Placental Abruption:
| Abruption | Definition | Management |
| Mild | Abruption with no fetal compromise |
|
| Moderate | Abruption with fetal compromise |
|
| Severe | Abruption with fetal death |
|

Retrieved July 5, 2023 from https://www.amboss.com/us/knowledge/antepartum-hemorrhage
Reference(s):
Society of Obstetricians and Gynecologists of Canada. ALARM Manual, 28th Ed. 2022.
| FHR Pattern (VEAL) | Cause (CHOP) | Management (MINE) | |||
| V | Variable Deceleration | C | Cord Compression | M | Maternal Repositioning |
| E | Early Deceleration | H | Head Compression | I | Identify Labour Progress |
| A | Acceleration | O | Okay! | N | No Intervention |
| L | Late Deceleration | P | Placental Insufficiency | E | Evaluate (reposition, fluids, oxygen, emergency delivery). |
Retrieved July 17, 2023, from Melbourne University Obstetrics and Gynecology Society (Facebook)
Norwitz E. R. (2022). Eclampsia. In Barss V (Ed.), UpToDate. Retrieved July 4, 2023, from https://www.uptodate.com/contents/eclampsia
|
Date and Time |
|
|---|---|
|
ID
|
CC
|
|
HPI: 4 Key Questions
|
Hx of Pregnancy
|
|
OBHx: Outcomes of previous pregnancies
|
|
|
PMHx
|
|
|
On Examination (O/E)
|
|
|
GxPx |
GTPAL |
|
G = Gravidity → total # of pregnancies |
G = Gravidity → total # of pregnancies
L = number of living children |
E.g., Patient has been pregnant 4 times. The first one ended in a miscarriage at 10 weeks, the second child was born healthy at 38 weeks, the third was carried to 23 weeks but was born stillborn and she is currently 35 weeks gestation with the fourth pregnancy.
This can be described as: G4P2 in GxPx format or G4T1P1A1L1 in the GTPAL format.
|
Assessing Contraction Pattern |
|||||||||||
|
Methods of Assessment |
|||||||||||
|
Palpation by Hand
|
Tocodynamometer (external)
|
Internal Intrauterine Pressure Catheter (IUPC)
|
|||||||||
|
Characteristics of Contractions |
|||||||||||
|
Frequency |
Duration |
Intensity |
Resting Tone |
||||||||
|
# of contractions in 10 minutes, averaged over 30 minutes Normal: ≤ 5 in 10 mins |
# of seconds from beginning to end of contraction Normal: <90 s |
Strength of contraction By palpation if using tocodynamometer: mild, moderate, or strong (strong = uterus cannot be indented) Normal (IUPC): 25-75 mmHg above baseline |
Firmness between contractions Palpation: soft or firm Normal (palpation): soft between contractions for at least 30s to allow for placental perfusion Normal (IUPC): 7-25 mmHg |
||||||||
|
Abnormal Contraction Pattern |
|||||||||||
|
Tachysystole - excessive uterine activity (commonly d/t exogenous augmentation by oxytocin or other uterotonic agent) Characteristics: >5 contractions per 10-min period averaged over 30 mins and/or Impact: Can reduce placental perfusion & result in fetal hypoxemia |
|||||||||||
Leopold Maneuvers: Systematic abdominal palpation maneuvers performed after 30-32 weeks gestation. They are used to determine the presentation, position, and engagement of the fetus in utero.
from Toronto Notes 2022
Fetal Orientation:
|
1. Fetal Lie: Relation of fetal long axis to long maternal uterus |
|
|
|
|
2. Presentation: The part of the fetus that overlies pelvic inlet (separation between abdominal & pelvic organs - borders include sacral promontory & pubic symphysis) |
|
|
Cephalic (head down in pelvic inlet) - most common Compound (more than one part presenting - e.g., cephalic or breech + extremity |
|
|
3. Fetal Position: Relationship to maternal pelvis |
|
|
Occiput Anterior (OA) - fetal occiput (posterior head) towards pubic symphysis (face down) |
|
|
4. Fetal Attitude: How much the fetal head flexes/extends during cephalic presentation |
|
|
Vertex - maximum flexion (most common) *spontaneous vaginal delivery possible in all attitudes |
|
|
5. Fetal Station: Measurement (in cm) of where the presenting part of the fetus is located in the pelvis, in relation to ischial spine |
|
|
Negative (-) = above ischial spine |
|
|
6. Synclitism: Parallelism between pelvic plane and plane of fetal head |
|
|
Synclitism - posture in which the 2 parietal bones are at the same level |
Choosing a Debrief Framework:
A good debrief has been identified in the literature as the most important part of a successful simulation experience. If you're a novice or inexperienced facilitator, use this table to help you choose which debrief framework you want to use, just tap the button on their name and you will be directed to the appropriate aids or scripts. While we recommend the PEARLS framework, take a look to see if there may be another that is a better fit for your situation.
|
|
|||||
|
Time |
Facilitator Level |
Prep Time |
Scenario Type |
Flexibility |
|
|
Moderate |
Novice |
Moderate |
Any |
High |
|
|
Short-Moderate |
Novice |
Low |
Short w/ Clear Objectives |
Low |
|
|
Moderate |
Novice |
Moderate |
Any, esp. Team-focused |
Moderate |
|
|
Very Short |
No experience |
None |
Any |
Low |
|
|
Short |
Novice |
Low |
Low number of non-technical skills |
Low |
|
|
Very Short |
No experience |
None |
Any |
Moderate |
|
|
Moderate-Long |
Novice |
Moderate |
Any |
Moderate |
(To learn more about this debriefing framework, visit our page on Debriefing resources)
If you need help with debriefing Crisis Resource Management skills, check out this infographic from Isaak & Stiegler: View Infographic
|
Phase |
Objective |
Task |
Sample Phrases |
||
|
1. Setting the Scene |
Create a safe context for learning |
State the goal of debriefing; articulate the basic assumption |
“Let’s spend X minutes debriefing. Our goal is to improve how we work together and care for our patients.” “Everyone here is intelligent and wants to improve”
|
||
|
2. Reactions |
Explore feelings |
Solicit initial reactions and emotions
|
“Any initial reactions?” “How are you feeling?” |
||
|
3. Description |
Clarify Facts |
Develop a shared understanding of the case |
“Can you please share a short summary of the case?” “What was the working diagnosis? Does everyone agree?”
|
||
|
4. Analysis |
Explore a variety of performance domains:
|
See bottom of guide for details on the analysis phase |
For each item to be debriefed: 1. Preview Statement: (to introduce topic)
2. Pick Analysis method + Analyze: (see below for more info on each method)
3. Mini Summary: (to summarize discussion of topic)
Phase Wrap-up: "Any outstanding issues or concerns before we start to close?" |
||
|
5. Application or Summary |
Identify take-aways |
Can be learner- or instructor-centered |
Learner-centered: “What are some takeaways from this discussion for our clinical practice?”
Instructor-centered: “The key learning points for the case were [insert learning points]”
|
||
|
Analysis Phase Details |
|||||
|
Choose an analysis approach (Different approaches can be used for different topics within the same analysis stage): |
|||||
|
Approach |
Objective |
Sample Phrases |
|||
|
Learner Self-Assessment
|
Promote reflection by asking learners to assess their own performance |
“What aspects were managed well and why?”
“What aspects do you want to change and why?”
|
|||
|
Focused Facilitation
|
Probe deeper on key aspects of performance, uncover mental frames guiding performance |
Use Advocacy-Inquiry Method Advocacy: "I saw [observation], I think [your point-of-view]” "I noticed [observation] I liked that/I was concerned..." Inquiry: “How do you see it? What were your thoughts at the time?” |
|||
|
Provide Information
|
Teach to close clear knowledge gaps as they emerge and provide directive feedback as needed |
“I noticed[behaviour]. Next time you may want to consider [suggested behaviour], because [rationale]” |
|||
PDF from debrief2learn.org: Here
Visual Guide: debrief2learn.org
Alternative Script: Here
Originally Created by: Bajaj K, Meguerdichian M, Thoma B, Huang S, Eppich W, Cheng A. The PEARLS Healthcare Debriefing Tool. Acad Med. 2018, 93(2), 336.
(To learn more about this debriefing framework, visit our page on Debriefing resources)
If you need help with debriefing Crisis Resource Management skills, check out this infographic from Isaak & Stiegler: View Infographic
|
Phase |
Goal |
Actions |
Possible Scripts |
|
Gather (Listen)
25% |
|
|
How do you feel? |
|
How do you think it went? Can you tell me what happened? |
||
|
Can anyone add anything to that account? |
||
|
Analyze (Guide Reflection)
50% |
|
|
I noticed… |
|
I noticed…. What was the thought process behind…. When….happened, I saw….What do you think….. I saw…I think….How do you see it? |
||
|
Tell me more about… How did you feel about…. I understand, but tell me about X aspect of the scenario |
||
|
Summarize (Help gather Conclusions)
25%
|
|
|
What are two things that you thought were effective or went well? |
|
What do you think are some areas you/your team need to work on? |
||
|
In today’s session, we…. Going forward, we should…. |
References/Adapted From:
(To learn more about this debriefing framework, visit our page on Debriefing resources)
If you need help with debriefing Crisis Resource Management skills, check out this infographic from Isaak & Stiegler: View Infographic
Instructions:
|
Actions |
Gather |
Analyze |
Summarize |
|
Closed-loop communication
Clear Messages
Clear Roles
Knowing one’s limitations
Knowledge Sharing
Constructive Intervention
Reevaluation and Summarizing
Mutual Respect
|
Student Observations
Instructor Observations
|
Done Well
Needs Improvement
|
Student-led Summary
Instructor-led Summary
|
References/Adapted from:
(To learn more about this debriefing framework, visit our page on Debriefing resources)
If you need help with debriefing Crisis Resource Management skills, check out this infographic from Isaak & Stiegler: View Infographic
|
|
Set learning objectives |
|
After Case |
How did it go? Address Concerns Review learning points Plan ahead |
Framework from:
(To learn more about this debriefing framework, visit our page on Debriefing resources)
If you need help with debriefing Crisis Resource Management skills, check out this infographic from Isaak & Stiegler: View Infographic
|
Diamond Debrief: Sample Phrases |
|
Description |
|
“So what happened?...and then what happened next?”
Continue asking until confident that the details of the scenario have been raised by the learners
“Let’s not judge our performance now, let’s just focus on what happened” |
|
Transition |
|
“This scenario was designed to show…”
“Let’s address technical and clinical questions. What is the protocol for…?”
“How do we normally deal with this clinical situation?”
“Everyone ok with that?” |
|
Analysis |
|
“How did that make you feel?” To participants, then group “Why?” Then use silence
“How did you/they do that exactly?” “Why did you respond in that way? “ or “Why did you take that action?”
“It feels like…was an issue. Did it feel like that to you?” What I’m hearing from you is…is that correct?”
“This is part of…” (identify the non-technical skill/human factor) “We refer to that as a human factor or non-technical skill, which means…” |
|
Transition |
|
“So, what we’ve talked about in this scenario is…” “What have we agreed we could do?” |
|
Application |
|
“What other kinds of situations might you face that might be similar? How are they similar?”
“How might these skills we discussed play out in those situations?”
“What are you going to do differently in your practice going forward?” |
|
Underlying Principles |
|
Description |
|
Reinforce a safe learning environment. Situate the debrief in the shared and meaningful activity that occurred. Keep the focus dispassionate—discuss what happened but avoid focus on emotions. Listen for emotional responses but resist the temptation to discuss emotions. Make sure everyone shares the same understanding of what happened.
|
|
Transition |
|
Transition into analysis by clarifying any technical and clinical issues |
|
Analysis |
|
Spend most of your time in Analysis. Deconstruct behaviours into specific actions, and explore what happened in detail. Ask about affective responses and validate them. Analyze and interpret the activity by applying appropriate frameworks or lenses (such as non-technical skills, or the clinical context surrounding the scenario). Keep discussion positive, and avoid the temptation to focus on “strengths and weaknesses”. Reflect responses back, allowing participants to amend or augment. |
|
Transition |
|
Transition into Application by reinforcing learning. |
|
Application |
|
Focus on moving from the specifics of the scenario to the more general world of practice. Break behaviours down into specific actions. Explore the other kinds of situations that these might apply to. Ask what participants will do differently in their practice. |
Adapted From: Jaye P, Thomas L, Reedy G (2015). 'The Diamond': a structure for simulation debrief. The Clinical Teacher 12(1). 171-175. onlinelibrary.wiley.com/doi/full/10.1111/tct.12300
If you need help with debriefing Crisis Resource Management skills, check out this infographic from Isaak & Stiegler: View Infographic
Pluses:
Deltas:
|
Plus (+) |
Delta (∆) |
References:
((To learn more about this debriefing framework, visit our page on Debriefing resources)
If you need help with debriefing Crisis Resource Management skills, check out this infographic from Isaak & Stiegler: View Infographic
|
Phase |
Purpose |
Process |
Sample Phrases |
|
Reactions |
|
|
How are you feeling? What are some initial reactions to what just happened? So, in that scenario… |
|
Analysis |
|
1. Observe an event or result. Comment on the observation.
2. Advocate for your position |
I saw that… I think… I noticed that…To me…
I saw…I’m concerned that… |
|
3. Investigate basis for learner’s thinking that led to the observed event or result |
What do you think? Why do you think that happened? How do you see it? What was the thought process behind….? |
||
|
4. Close the gap through discussion and didactics |
I hear…. What would it take for you to do this next time? How could we do this differently next time? I think a few good ideas that came up were… I’d like to say a little bit about…from my experience/literature |
||
|
Summary |
|
|
What are some takeaways from today? What went well today? What would you do differently next time?
In today’s session, we…. Going forward, we should… |
Adapted from:
Assessment:
Fetal Heart Rate Monitoring:
Shock and Massive Hemorrhage Protocol: