Learners will manage a high-risk delivery of a breech presentation when transportation to an urban centre is unavailable.
It’s mid-January and there is a massive snowstorm outside. One of the nurses looks at you and says, “It’s supposed to be like this all day. I think it’s about -25 degrees Celsius.” You’ve had a quiet morning but days like this make you uneasy knowing how dangerous the highway can get.
You’re working in a rural 1A maternity site (no local cesarean section capabilities), and the nearest urban centre is 400 km away. A 21 y/o woman presents to the ED alone at approximately 37 weeks gestation. She’s had infrequent antenatal care visits. The last visit confirmed breech presentation despite attempted external cephalic rotation. She did not want to leave the community for the birth. She has been feeling something “leaking” since 4:00 AM this morning.
She has no known allergies, her family history and past medical history are insignificant, and her general physical exam is otherwise normal.
On examination, the infant will be in breech presentation and the learner must deliver the fetus using various manual maneuvers while addressing the barriers to transportation in a rural community. There is also a five-minute extension to practice active management of the third stage of labour.
This simulation is part of ØRECLESS (Rural Emergencies and Complications in Labour Events Simulations Suite).
Overall Goal: Manage a high-risk delivery of a breech presentation when transportation to an urban centre is unavailable.
Specific Learning Objectives:
Time Recommended: 60 minutes total (10 min Setup | 20 min Scenario | 30 min Debrief)
Patient Recommendation: Standardized Patient + OB Mannequin + OB Trainer
Medical Equipment:
Medications:
Other:
|
This SIM requires one learner. Supporting roles can (1) be assigned to complete tasks by the learner, (2) provide assistance with maneuvers, and (3) provide statements throughout the SIM to allow for progression through the stages.
|
Moulage: Task trainer set up with the fetus in complete breech presentation, left sacrum posterior position, and fetal station of 0.
Set-Up: The woman should walk into the ED alone and concerned.
Note: While prepping for your simulation, don't forget to prep for the debrief. Become comfortable with your chosen framework, review your objectives. For additional debriefing resources, see our Resources page.
Original Author: Tiana Bressan
Originally published on: October 29, 2023
Most Recent Modification: November 3, 2023
A good prebriefing is an essential component of running effective simulations, as it sets the stage for everything that comes after it1-3. An effective prebrief will create a safe container for learning, and in doing so, help participants feel more comfortable pushing their limits, sharing their thoughts and feelings, and buying into the experience. In turn, this will enhance engagement, participation, and learning. To that end, the prebriefing process needs to cover a lot of information1-5, which can make it daunting to novice or non-expert facilitators. To help, we have consulted the relevant literature and put together a prebrief guide to ensure that you have the tools you need to run an effective pre-briefing session.
Throughout the pre-brief, it is important that you convey your commitment to respecting learners and their perspective2-4, and establish and maintain the simulation as a safe space for learning1,4,5.
Prebrief Guide (Sample Phrases in Italics)
Welcome learners. Introduce yourself, your role, and your experience with simulation.
Go over the time requirements for the simulation, when breaks will occur, how learners should handle incoming calls or texts, etc.
Clarify the learning objectives for the simulation1-5. Give information on the purpose of the simulation without giving out specific actions or information that might compromise the learning experience for participants.
Explain how participants will be evaluated (formative/summative/not evaluated). Briefly discuss the debrief process that will take place at the end of the simulation.
Give details on what expectations are for the learners' behaviour during the simulation, setting basic ground rules2-5. Go over expectations for yourself as the facilitator. Reinforce the simulation as a learning environment, where mistakes aren't something to be punished but opportunities for further learning.
This could be a good place to pause and ask learners if they have any additional expectations, fears, comments, or questions about the topic for the day.
Ensure all participants agree to the confidentiality expectations of the simulation. Often, this will follow the mantra of "What happens in the simulation stays in the simulation," where learners and instructors agree not to share information on others' performance or scenario details outside of the simulation environment.
Explain that you've done what you can to make the simulation as real as possible, but acknowledge the limitations. Ask the learner to commit to doing what they can to act as if everything was real, explaining that the quality of their learning will depend on their willingness to participate as fully as possible. For the first simulation with a new group, it could be helpful to explain the importance of a mutual fiction contract.
Explain the different roles in the simulation and assign learners to them. If you have predetermined scripts for certain roles, hand them out here.
Explain the resources that will be available for the participants to use, how they should call for help in the simulation, what your role will be in providing information.
Orient participants to simulation space, equipment, manikin, etc. This can also be done by allowing participants to explore the simulation space and manikin for themselves.
Ask for questions!
References
1. Rudolph JW, Raemer DB, Simon R. Establishing a safe container for learning in simulation: the role of the presimulation briefing. Simul Healthc. 2014 Dec;9(6):339-49. doi: 10.1097/SIH.0000000000000047. PMID: 25188485.
2. Leigh G, Steuben F. Setting Learners up for Success: Presimulation and Prebriefing Strategies. Teaching and Learning in Nursing. 2018; 13(3):185-189. https://doi.org/10.1016/j.teln.2018.03.004
3. Lecomte F, Jaffrelot M. Chapter 33 - Prebriefing and Briefing. Clinical Simulation. 2019; 2nd ed.; 471-482. https://doi.org/10.1016/B978-0-12-815657-5.00034-6.
4. INACSL Standards Committee (2016, December). INACSL standards of best practice: SimulationSM Facilitation. Clinical Simulation in Nursing, 12(S), S16-S20. http://dx.doi.org/10.1016/j.ecns.2016.09.007.
5. Simon R, Raemer D, Rudolph J. Rater's handbook for the Debriefing Assessment for Simulation in Healthcare (DASH) Rater Version. 2009. http://www.harvardmedsim.org/debriefing-assesment-simulation-healthcare.php.
It’s mid-January and there is a massive snowstorm outside. One of the nurses looks at you and says, “It’s supposed to be like this all day. I think it’s about -25 degrees Celsius.” You’ve had a quiet morning but days like this make you uneasy knowing how dangerous the highway can get.
You’re working in a rural 1A maternity site (no local cesarean section capabilities) and the nearest urban centre is 400 km away. A 21 y/o woman presents to the ED alone at approximately 37 weeks gestation. She’s had infrequent antenatal care visits. The last visit confirmed breech presentation despite attempted external cephalic rotation. She did not want to leave the community for the birth. She has been feeling something “leaking” since 4:00 AM this morning.
She has no known allergies, her family history and past medical history are insignificant, and her general physical exam is otherwise normal.
|
Patient Chart |
||||||||||
|
Name: Josephine Lefèvre |
Age: 21 |
Gender: F |
Weight: 82.3 kg |
Height: 162 cm |
GA: 37 Weeks |
|||||
|
Temp: 37.1 |
HR: 110 bpm |
BP: 135/95 |
RR: 26/min |
O2Sat: 99% |
GCS: 15 |
|||||
| Presenting complaint: Clear, liquid vaginal discharge since 4:00 AM this morning. | ||||||||||
A 21 y/o woman is presenting to the ED alone, appearing to be full-term, and stating that she has been "feeling something leaking."
Modifiers (in red): Actions by the learner (which will have a consequence) OR actions to prompt learner. Extra information, audio clips, etc. are provided below.
| Patient Vitals | ||||
| BP: 135/95 | HR (Rhythm): 110 bpm (Sinus Tachycardia) | RR: 26/min. | ||
| O2SAT: 99% | Temperature: 37.1 degrees Celsius | GCS: 15 | ||
| Expected Learner Actions |
|---|
|
Call nursing/staff to increase available team numbers |
| 8 min. OR Actions Complete ⇒ 2. Transportation |
Pronouns: She/her
Pregnancy Records: Incomplete - see information below.
Gestation: 37 Weeks
Membrane: Ruptured, clear fluid
No. previous deliveries: Nulliparous
Pregnancy Complications:
Medication(s): None.
Other: No Allergies. Insignificant family history and past medical history.
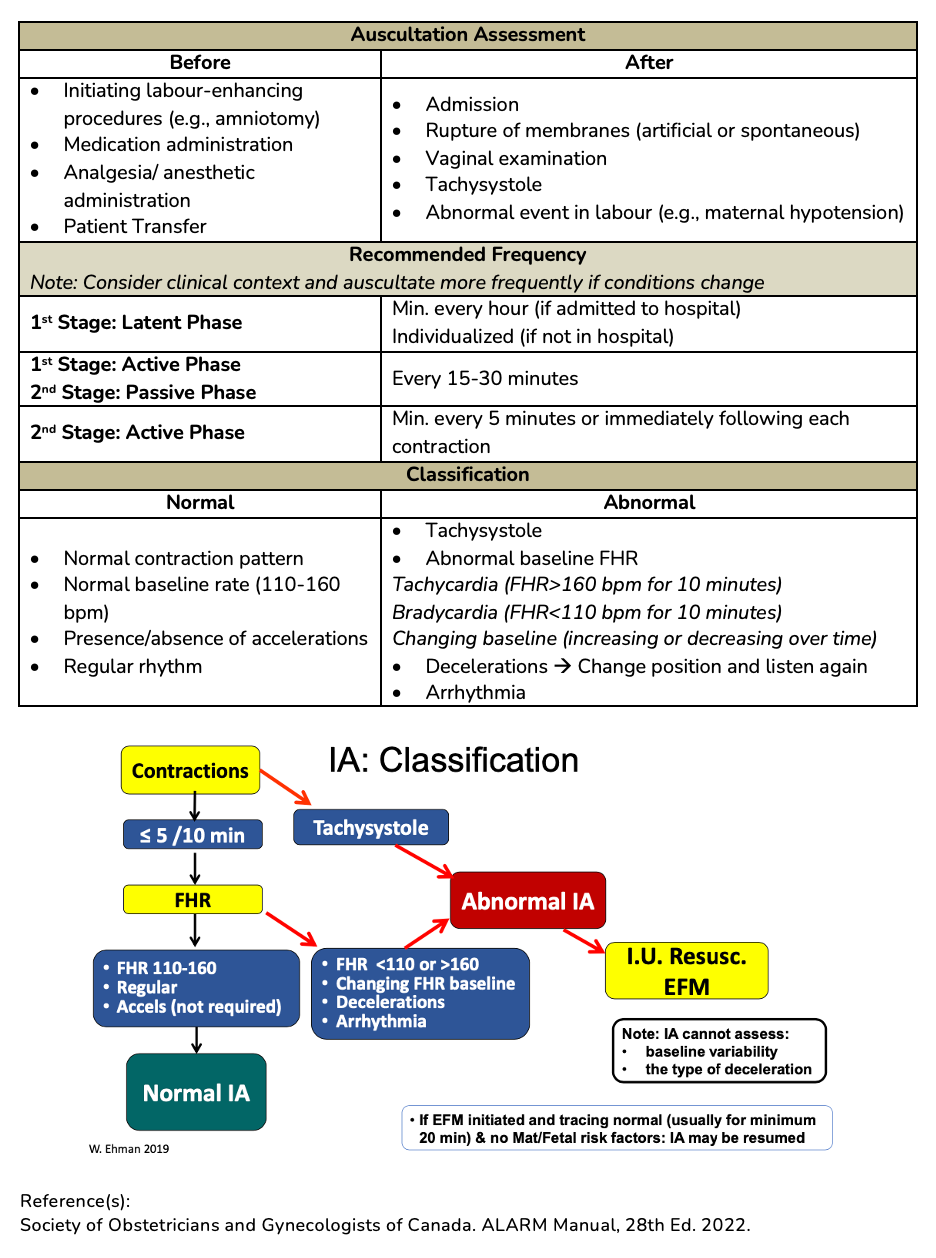
Baseline FHR: https://drive.google.com/file/d/1R66RLkfzAEFMecR7QZQeKYeGOeEyIDnq/view?usp=share_link
Post-Contraction: https://drive.google.com/file/d/1R66RLkfzAEFMecR7QZQeKYeGOeEyIDnq/view?usp=share_link
FHR = 150 bpm
Rhythm: Regular
HR heard above the maternal umbilicus.
No appreciable accelerations or decelerations.
General Abdominal Exam: No visible asymmetry, lesions, or scars. No appreciable masses, swelling, rigidity, or guarding. Woman is full-term.
Leopold Maneuvers:
Fundal Grip: Head is palpable at the uterine fundus.
Lateral Grip: Fetal back is on the left side and the limbs are felt on the right.
Pelvic Grip: Palpable soft, irregular mass.
Fetal Lie: Longitudinal
Fetal Presentation: Complete Breech
Position: Left Sacrum Posterior (LSP)
Uterine Activity Characteristics:
Frequency: Every 4 min. (~2 contractions/ 10 minutes)
Duration: 65 sec.
Intensity: Strong
Resting tone: Soft between contractions
Dilation: 5cm
Fetal Station: 0
Effacement: 80%
Membrane: Absent
Palpable fetal buttocks. Umbilical cord prolapse and significant pelvic contraction are ruled out.
Breech presentation has been identified. Assess transportation options to send the woman to the nearest urban centre.
Modifiers (in red): Actions by the learner (which will have a consequence) OR actions to prompt learner. Extra information, audio clips, etc. are provided below.
| Expected Learner Actions |
|---|
|
Initiate contact with referral centre specialist (e.g., Ontario - Criticall) |
| 5 min. OR Actions Complete ⇒ 3. Delivery |
The woman is now in screaming pain, "I need to push!" The woman's contractions weaken and labour must be sped up. Practice proper medication administration and management of this delivery complication.
Modifiers (in red): Actions by the learner (which will have a consequence) OR actions to prompt learner. Extra information, audio clips, etc. are provided below.
| Expected Learner Actions |
|---|
|
No action (in 1 min.) ⇒ Nurse: "How much oxytocin should I give to help with contractions? Should we keep her in this position?" |
| 5 min. OR Actions Complete ⇒ 4. Delivery of Placenta |
Dilation: ~3 cm (size of a banana slice)
Fetal Station: -2
Effacement: 80%
Copious vaginal blood.
Dilation: ~3 cm (size of a banana slice)
Fetal Station: -2
Effacement: 80%
Copious vaginal blood.
The neonate has been successfully delivered and handed to the woman for skin-to-skin contact. At one minute, the neonate is crying and has a normal appearance, pulse of 120, and normal muscle tone. Maternal vitals are normal. There is no maternal or fetal trauma. Continue with delivery of the placenta.
Modifiers (in red): Actions by the learner (which will have a consequence) OR actions to prompt learner. Extra information, audio clips, etc. are provided below.
| Expected Learner Actions |
|---|
|
Cord Clamping Facilitator selects Option 1 or proceeds to 5. Case Complete: |
| 2 min. OR Actions Complete ⇒ 5. Case Complete. |
The cord is lengthening and the uterus is becoming firmer. The placenta was delivered, has been inspected, and the case is complete.

Retrieved July 2, 2023 from: https://www.parents.com/pregnancy/giving-birth/labor-and-delivery/cervix-dilation-chart-pictures-that-explain-the-stages-of-labor/

Retrieved July 27, 2023 from: https://www.instagram.com/p/CHJCbAhgdIu/?utm_source=ig_web_button_share_sheet
Retrieved July 27, 2023 from: https://www.youtube.com/watch?v=x17vY7_3M2M

Adapted September 12, 2023 from https://www.medicalnewstoday.com/articles/326380
|
Apgar Score |
||||
|
Indicator |
0 Points |
1 Point |
2 Points |
|
|
A |
Activity (Muscle Tone) |
Absent |
Some tone and flexion |
Active motion with flexed muscle tone |
|
P |
Pulse |
Absent |
Less than 100bpm |
100+ bpm |
|
G |
Grimace (Reflex irritability) |
Floppy, No response to stimulation |
Grimacing |
Cries, coughs, or sneezes |
|
A |
Appearance (Skin Color) |
Pale or blue |
Pink but blue extremities |
Entirely pink |
|
R |
Respiration |
Absent |
Slow, irregular, weak, or gasping |
Crying vigorously |
|
Total Score: |
||||
Created using information from: Simon LV, Hashmi MF, Bragg BN. APGAR Score. StatPearls. 2022 Feb. https://www.ncbi.nlm.nih.gov/books/NBK470569/
| Signs of Placental Separation | |
|
1. Gush of blood |
|
| Active Management | |
|
|
Drug Name |
Characteristics |
Side Effects |
PPH Usage |
|
|
Medication Class: Oxytocics |
||||
|
Oxytocin |
Preferred first line uterotonic Stimulates muscle of upper uterine segment causing contraction to compress blood vessels IV: acts immediately IM: 3-5 minutes |
Rare: nausea, vomiting, headache, flushing Never give as IV bolus → hypotension, tachycardia & potential cardiovascular collapse possible Water intoxication with high doses, prolonged infusion, or hypotonic IV solution → Use normal saline or Ringers Lactate |
Prevention Vaginal Delivery:
Cesarean (elective):
Cesarean (intrapartum):
Treatment: 20-40 IU in 1000 mL normal saline, initially wide open |
|
|
Carbetocin |
Long-acting oxytocin analogue Alternative agent if oxytocin is not available or consider if pt. is at high risk of PPH |
Nausea, vomiting, flushing, headache |
Prevention Vaginal Delivery: 100 mcg IM Cesarean: 100 mcg over ≥ 30 seconds Treatment: Limited data available |
|
|
Medication Class: Ergot Alkaloids |
||||
|
Ergot Alkaloids |
Stimulates myometrium of upper AND lower uterine segments IM: 2-5 minutes IV: acts <1 minute (however, IV not recommended) |
Nausea, vomiting, hypertension Contraindicated in all hypertensive disorders of pregnancy |
Prevention: 0.2-0.25 mg IM Treatment: 0.2-0.25 mg IM (may repeat at 2h intervals) |
|
|
Medication Class: Prostaglandins |
||||
|
Misoprostol |
Prostaglandin E1 Causes vasoconstriction & enhanced contractility of the myometrium |
Fever (most common with >600 mcg) |
Prevention: 400 mcg SL (SL achieves highest serum peak level) Treatment |
|
|
Carboprost |
Prostaglandin F2α Causes vasoconstriction & enhanced contractility of myometrium |
Vomiting, diarrhea, fever, bronchospasm Use with extreme caution if asthma or major cardiovascular, renal, or hepatic dysfunction) |
Treatment |
|
|
Medication Class: Tranexamic Acid |
||||
|
Tranexamic Acid |
Not a uterotonic Inhibits fibrinolysis Consider in pt. at very high risk of PPH |
N/A |
Prevention Vaginal Delivery: 1 g IV over 10 minutes within 10 minutes after vaginal delivery Cesarean: 1 g IV over 10 minutes before skin incision Treatment |
|
Reference(s):
Society of Obstetricians and Gynecologists of Canada. ALARM Manual, 28th Ed. 2022.
|
Contraindications to planned vaginal delivery breech. |
|
Contraindications to planned vaginal delivery breech.
|
|
Breech Delivery Technique Notes |
|
Delivery Technique
In the rare circumstance of a trapped aftercoming head or irreducible nuchal arms perform a symphysiotomy or Zavanelli maneuver. |
Reference(s):
Society of Obstetricians and Gynecologists of Canada. ALARM Manual, 28th Ed. 2022.
|
Pinard’s Maneuver: deliver fetal legs once the popliteal fossae are visible.
1. Insert two fingers along one leg to the knee. Note: The knees of a frank breech are hyperextended at this point. It is important to correctly identify the popliteal fossae to avoid further hyperextension and damage to the fetal knee. |
|
Bracht’s Maneuver: suprapubic pressure with the extension of the fetal neck.
|
|
Bickenbach Maneuver: reduction of the nuchal arms.
Release of the posterior arm. Release of the anterior arm. |
|
Løvset’s Maneuver: reduction of the nuchal arms.
Release of the posterior arm. Release of the first arm brings the other arm posteriorly. |
|
Mauriceau-Smellie-Veit Maneuver: delivery of the aftercoming head.
Note: As the fetal head is being delivered, flexion of the head is maintained by suprapubic pressure provided by an assistant, and simultaneously by pressure on the maxilla (inset) by the operator as traction is applied. |
|
Piper forceps: delivery of the aftercoming head.
Note: The blue arrows show the direction of movement. The fetal body is elevated using a warm towel and the left blade of the forceps is applied to the aftercoming head. The right blade is applied with the body still elevated. |
Videos:
Breech Delivery Technique (4 min): https://youtu.be/d9pU_6LDVUM
In-depth Technique Explanations (12 min) – Includes Piper Forceps Delivery: https://youtu.be/xOqWT06qVS8
Reference(s):
Society of Obstetricians and Gynecologists of Canada. ALARM Manual, 28th Ed. 2022.
Brandt-Andrews Maneuver (preferred): an abdominal hand secures the uterine fundus to hold it in a fixed position and prevent uterine inversion while the other hand exerts sustained downward traction on the clamped umbilical cord.
Reference(s):
Anderson, Janice M, and Duncan Etches. 2007. Prevention and Management of Postpartum Hemorrhage. www.aafp.org/afp. (October 12, 2023).

Important Notes Regarding Pharmacological use in Labour:
Options for Pharmacological Pain Management in Labour (see dosing information below):
Suggested Opioid use in labour:
|
Stage of Labour |
Nulliparous |
Parous |
|
Latent Stage: |
IM/SC Morphine |
IM/SC Morphine |
|
Early Active Stage: |
IM/SC or IV Morphine |
IV Morphine or Fentanyl |
|
Late Active Stage: |
IV Morphine or Fentanyl |
IV Fentanyl |
|
Second Stage: |
IV Fentanyl |
IV Fentanyl |
Reference(s):
Grant G. (2022). Pharmacologic management of pain during labor and delivery. In Crowley M (Ed.), UpToDate. Retrieved Jul 2, 2023, from https://www.uptodate.com/contents/pharmacologic-management-of-pain-during-labor-and-delivery
Society of Obstetricians and Gynecologists of Canada. ALARM Manual, 28th Ed. 2022.
|
Date and Time |
|
|---|---|
|
ID
|
CC
|
|
HPI: 4 Key Questions
|
Hx of Pregnancy
|
|
OBHx: Outcomes of previous pregnancies
|
|
|
PMHx
|
|
|
On Examination (O/E)
|
|
|
GxPx |
GTPAL |
|
G = Gravidity → total # of pregnancies |
G = Gravidity → total # of pregnancies
L = number of living children |
E.g., Patient has been pregnant 4 times. The first one ended in a miscarriage at 10 weeks, the second child was born healthy at 38 weeks, the third was carried to 23 weeks but was born stillborn and she is currently 35 weeks gestation with the fourth pregnancy.
This can be described as: G4P2 in GxPx format or G4T1P1A1L1 in the GTPAL format.
|
Assessing Contraction Pattern |
|||||||||||
|
Methods of Assessment |
|||||||||||
|
Palpation by Hand
|
Tocodynamometer (external)
|
Internal Intrauterine Pressure Catheter (IUPC)
|
|||||||||
|
Characteristics of Contractions |
|||||||||||
|
Frequency |
Duration |
Intensity |
Resting Tone |
||||||||
|
# of contractions in 10 minutes, averaged over 30 minutes Normal: ≤ 5 in 10 mins |
# of seconds from beginning to end of contraction Normal: <90 s |
Strength of contraction By palpation if using tocodynamometer: mild, moderate, or strong (strong = uterus cannot be indented) Normal (IUPC): 25-75 mmHg above baseline |
Firmness between contractions Palpation: soft or firm Normal (palpation): soft between contractions for at least 30s to allow for placental perfusion Normal (IUPC): 7-25 mmHg |
||||||||
|
Abnormal Contraction Pattern |
|||||||||||
|
Tachysystole - excessive uterine activity (commonly d/t exogenous augmentation by oxytocin or other uterotonic agent) Characteristics: >5 contractions per 10-min period averaged over 30 mins and/or Impact: Can reduce placental perfusion & result in fetal hypoxemia |
|||||||||||
Leopold Maneuvers: Systematic abdominal palpation maneuvers performed after 30-32 weeks gestation. They are used to determine the presentation, position, and engagement of the fetus in utero.
from Toronto Notes 2022
Fetal Orientation:
|
1. Fetal Lie: Relation of fetal long axis to long maternal uterus |
|
|
|
|
2. Presentation: The part of the fetus that overlies pelvic inlet (separation between abdominal & pelvic organs - borders include sacral promontory & pubic symphysis) |
|
|
Cephalic (head down in pelvic inlet) - most common Compound (more than one part presenting - e.g., cephalic or breech + extremity |
|
|
3. Fetal Position: Relationship to maternal pelvis |
|
|
Occiput Anterior (OA) - fetal occiput (posterior head) towards pubic symphysis (face down) |
|
|
4. Fetal Attitude: How much the fetal head flexes/extends during cephalic presentation |
|
|
Vertex - maximum flexion (most common) *spontaneous vaginal delivery possible in all attitudes |
|
|
5. Fetal Station: Measurement (in cm) of where the presenting part of the fetus is located in the pelvis, in relation to ischial spine |
|
|
Negative (-) = above ischial spine |
|
|
6. Synclitism: Parallelism between pelvic plane and plane of fetal head |
|
|
Synclitism - posture in which the 2 parietal bones are at the same level |
Compress the uterus against the anterior part of the cervix with a hand in the vagina and a hand on the fundus.

Retrieved July 20, 2023 from Bromberek, Elaine & Smereck, Janet. (2017). Evaluation and Treatment of Postpartum Hemorrhage. 10.1007/978-3-319-54410-6_8.
Choosing a Debrief Framework:
A good debrief has been identified in the literature as the most important part of a successful simulation experience. If you're a novice or inexperienced facilitator, use this table to help you choose which debrief framework you want to use, just tap the button on their name and you will be directed to the appropriate aids or scripts. While we recommend the PEARLS framework, take a look to see if there may be another that is a better fit for your situation.
|
|
|||||
|
Time |
Facilitator Level |
Prep Time |
Scenario Type |
Flexibility |
|
|
Moderate |
Novice |
Moderate |
Any |
High |
|
|
Short-Moderate |
Novice |
Low |
Short w/ Clear Objectives |
Low |
|
|
Moderate |
Novice |
Moderate |
Any, esp. Team-focused |
Moderate |
|
|
Very Short |
No experience |
None |
Any |
Low |
|
|
Short |
Novice |
Low |
Low number of non-technical skills |
Low |
|
|
Very Short |
No experience |
None |
Any |
Moderate |
|
|
Moderate-Long |
Novice |
Moderate |
Any |
Moderate |
(To learn more about this debriefing framework, visit our page on Debriefing resources)
If you need help with debriefing Crisis Resource Management skills, check out this infographic from Isaak & Stiegler: View Infographic
|
Phase |
Objective |
Task |
Sample Phrases |
||
|
1. Setting the Scene |
Create a safe context for learning |
State the goal of debriefing; articulate the basic assumption |
“Let’s spend X minutes debriefing. Our goal is to improve how we work together and care for our patients.” “Everyone here is intelligent and wants to improve”
|
||
|
2. Reactions |
Explore feelings |
Solicit initial reactions and emotions
|
“Any initial reactions?” “How are you feeling?” |
||
|
3. Description |
Clarify Facts |
Develop a shared understanding of the case |
“Can you please share a short summary of the case?” “What was the working diagnosis? Does everyone agree?”
|
||
|
4. Analysis |
Explore a variety of performance domains:
|
See bottom of guide for details on the analysis phase |
For each item to be debriefed: 1. Preview Statement: (to introduce topic)
2. Pick Analysis method + Analyze: (see below for more info on each method)
3. Mini Summary: (to summarize discussion of topic)
Phase Wrap-up: "Any outstanding issues or concerns before we start to close?" |
||
|
5. Application or Summary |
Identify take-aways |
Can be learner- or instructor-centered |
Learner-centered: “What are some takeaways from this discussion for our clinical practice?”
Instructor-centered: “The key learning points for the case were [insert learning points]”
|
||
|
Analysis Phase Details |
|||||
|
Choose an analysis approach (Different approaches can be used for different topics within the same analysis stage): |
|||||
|
Approach |
Objective |
Sample Phrases |
|||
|
Learner Self-Assessment
|
Promote reflection by asking learners to assess their own performance |
“What aspects were managed well and why?”
“What aspects do you want to change and why?”
|
|||
|
Focused Facilitation
|
Probe deeper on key aspects of performance, uncover mental frames guiding performance |
Use Advocacy-Inquiry Method Advocacy: "I saw [observation], I think [your point-of-view]” "I noticed [observation] I liked that/I was concerned..." Inquiry: “How do you see it? What were your thoughts at the time?” |
|||
|
Provide Information
|
Teach to close clear knowledge gaps as they emerge and provide directive feedback as needed |
“I noticed[behaviour]. Next time you may want to consider [suggested behaviour], because [rationale]” |
|||
PDF from debrief2learn.org: Here
Visual Guide: debrief2learn.org
Alternative Script: Here
Originally Created by: Bajaj K, Meguerdichian M, Thoma B, Huang S, Eppich W, Cheng A. The PEARLS Healthcare Debriefing Tool. Acad Med. 2018, 93(2), 336.
(To learn more about this debriefing framework, visit our page on Debriefing resources)
If you need help with debriefing Crisis Resource Management skills, check out this infographic from Isaak & Stiegler: View Infographic
|
Phase |
Goal |
Actions |
Possible Scripts |
|
Gather (Listen)
25% |
|
|
How do you feel? |
|
How do you think it went? Can you tell me what happened? |
||
|
Can anyone add anything to that account? |
||
|
Analyze (Guide Reflection)
50% |
|
|
I noticed… |
|
I noticed…. What was the thought process behind…. When….happened, I saw….What do you think….. I saw…I think….How do you see it? |
||
|
Tell me more about… How did you feel about…. I understand, but tell me about X aspect of the scenario |
||
|
Summarize (Help gather Conclusions)
25%
|
|
|
What are two things that you thought were effective or went well? |
|
What do you think are some areas you/your team need to work on? |
||
|
In today’s session, we…. Going forward, we should…. |
References/Adapted From:
(To learn more about this debriefing framework, visit our page on Debriefing resources)
If you need help with debriefing Crisis Resource Management skills, check out this infographic from Isaak & Stiegler: View Infographic
Instructions:
|
Actions |
Gather |
Analyze |
Summarize |
|
Closed-loop communication
Clear Messages
Clear Roles
Knowing one’s limitations
Knowledge Sharing
Constructive Intervention
Reevaluation and Summarizing
Mutual Respect
|
Student Observations
Instructor Observations
|
Done Well
Needs Improvement
|
Student-led Summary
Instructor-led Summary
|
References/Adapted from:
(To learn more about this debriefing framework, visit our page on Debriefing resources)
If you need help with debriefing Crisis Resource Management skills, check out this infographic from Isaak & Stiegler: View Infographic
|
|
Set learning objectives |
|
After Case |
How did it go? Address Concerns Review learning points Plan ahead |
Framework from:
(To learn more about this debriefing framework, visit our page on Debriefing resources)
If you need help with debriefing Crisis Resource Management skills, check out this infographic from Isaak & Stiegler: View Infographic
|
Diamond Debrief: Sample Phrases |
|
Description |
|
“So what happened?...and then what happened next?”
Continue asking until confident that the details of the scenario have been raised by the learners
“Let’s not judge our performance now, let’s just focus on what happened” |
|
Transition |
|
“This scenario was designed to show…”
“Let’s address technical and clinical questions. What is the protocol for…?”
“How do we normally deal with this clinical situation?”
“Everyone ok with that?” |
|
Analysis |
|
“How did that make you feel?” To participants, then group “Why?” Then use silence
“How did you/they do that exactly?” “Why did you respond in that way? “ or “Why did you take that action?”
“It feels like…was an issue. Did it feel like that to you?” What I’m hearing from you is…is that correct?”
“This is part of…” (identify the non-technical skill/human factor) “We refer to that as a human factor or non-technical skill, which means…” |
|
Transition |
|
“So, what we’ve talked about in this scenario is…” “What have we agreed we could do?” |
|
Application |
|
“What other kinds of situations might you face that might be similar? How are they similar?”
“How might these skills we discussed play out in those situations?”
“What are you going to do differently in your practice going forward?” |
|
Underlying Principles |
|
Description |
|
Reinforce a safe learning environment. Situate the debrief in the shared and meaningful activity that occurred. Keep the focus dispassionate—discuss what happened but avoid focus on emotions. Listen for emotional responses but resist the temptation to discuss emotions. Make sure everyone shares the same understanding of what happened.
|
|
Transition |
|
Transition into analysis by clarifying any technical and clinical issues |
|
Analysis |
|
Spend most of your time in Analysis. Deconstruct behaviours into specific actions, and explore what happened in detail. Ask about affective responses and validate them. Analyze and interpret the activity by applying appropriate frameworks or lenses (such as non-technical skills, or the clinical context surrounding the scenario). Keep discussion positive, and avoid the temptation to focus on “strengths and weaknesses”. Reflect responses back, allowing participants to amend or augment. |
|
Transition |
|
Transition into Application by reinforcing learning. |
|
Application |
|
Focus on moving from the specifics of the scenario to the more general world of practice. Break behaviours down into specific actions. Explore the other kinds of situations that these might apply to. Ask what participants will do differently in their practice. |
Adapted From: Jaye P, Thomas L, Reedy G (2015). 'The Diamond': a structure for simulation debrief. The Clinical Teacher 12(1). 171-175. onlinelibrary.wiley.com/doi/full/10.1111/tct.12300
If you need help with debriefing Crisis Resource Management skills, check out this infographic from Isaak & Stiegler: View Infographic
Pluses:
Deltas:
|
Plus (+) |
Delta (∆) |
References:
((To learn more about this debriefing framework, visit our page on Debriefing resources)
If you need help with debriefing Crisis Resource Management skills, check out this infographic from Isaak & Stiegler: View Infographic
|
Phase |
Purpose |
Process |
Sample Phrases |
|
Reactions |
|
|
How are you feeling? What are some initial reactions to what just happened? So, in that scenario… |
|
Analysis |
|
1. Observe an event or result. Comment on the observation.
2. Advocate for your position |
I saw that… I think… I noticed that…To me…
I saw…I’m concerned that… |
|
3. Investigate basis for learner’s thinking that led to the observed event or result |
What do you think? Why do you think that happened? How do you see it? What was the thought process behind….? |
||
|
4. Close the gap through discussion and didactics |
I hear…. What would it take for you to do this next time? How could we do this differently next time? I think a few good ideas that came up were… I’d like to say a little bit about…from my experience/literature |
||
|
Summary |
|
|
What are some takeaways from today? What went well today? What would you do differently next time?
In today’s session, we…. Going forward, we should… |
Adapted from:
Assessment:
Fetal Heart Rate Monitoring:
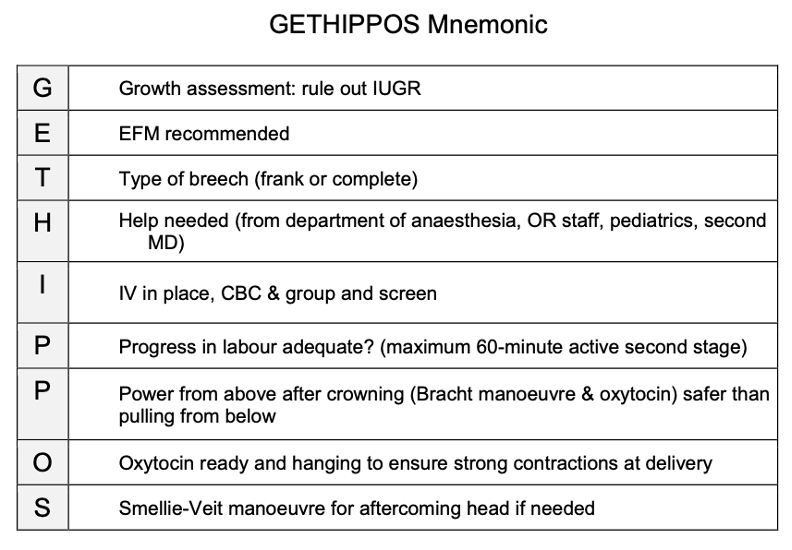
Breech Management:
Third Stage of Labour: